
Clinical history
64-year-old female generally fit and well. Previously involved in a road traffic collision and treated at a major trauma centre. She sustained a comminuted intra-articular distal humerus fracture that was managed operatively with open reduction and internal fixation.
She later presented to clinic with complaints of stiffness, swelling, and persistent pain around the elbow. Radiographs demonstrated failure of the original fixation with fragment displacement, loss of joint congruency, metaphyseal non-union, and the presence of heterotopic ossifications (HOs). The combination of clinical and radiological findings raised suspicion for infection. Neurovascular examination was normal, and there was no sinus formation.
Treatment
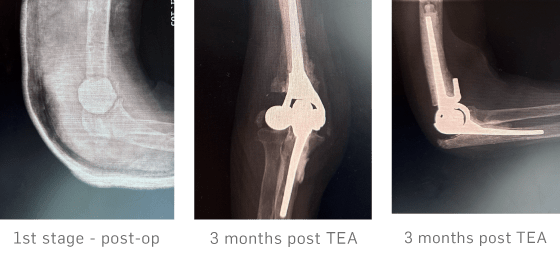
A staged surgical approach was adopted. Stage 1 involved removal of all metalwork, multiple tissue and bone samples for microbiological analysis, extensive debridement of necrotic bone and heterotopic ossifications, thorough lavage, and insertion of an antibiotic-loaded cement spacer along with 10 cc of STIMULAN mixed with antibiotic and made into beads. The patient commenced empiric intravenous antibiotics via a PICC line, which were continued for two weeks until culture results confirmed no bacterial growth.
After a 3 month interval, Stage 2 was performed, consisting of a total elbow arthroplasty (TEA).
Outcome
At the 3 month post-operative review, radiographs showed complete resorption of the STIMULAN beads and satisfactory integration of the prosthesis without evidence of loosening or subsidence. Clinically, the surgical scar was well healed, with restoration of functional, pain-free elbow movements. The patient reported marked improvement compared with her preoperative status, and there were no clinical or radiological signs of infection.
Note: See STIMULAN page for regulatory statements. MA0561R1
Listed below are 4 of the most relevant articles for this piece but there is much more to explore on our Library page.
Explore Library